Gut Health Made Practical: Restore Your Balance
Gut Health Made Practical for Injury Recovery: A Guide

Overview
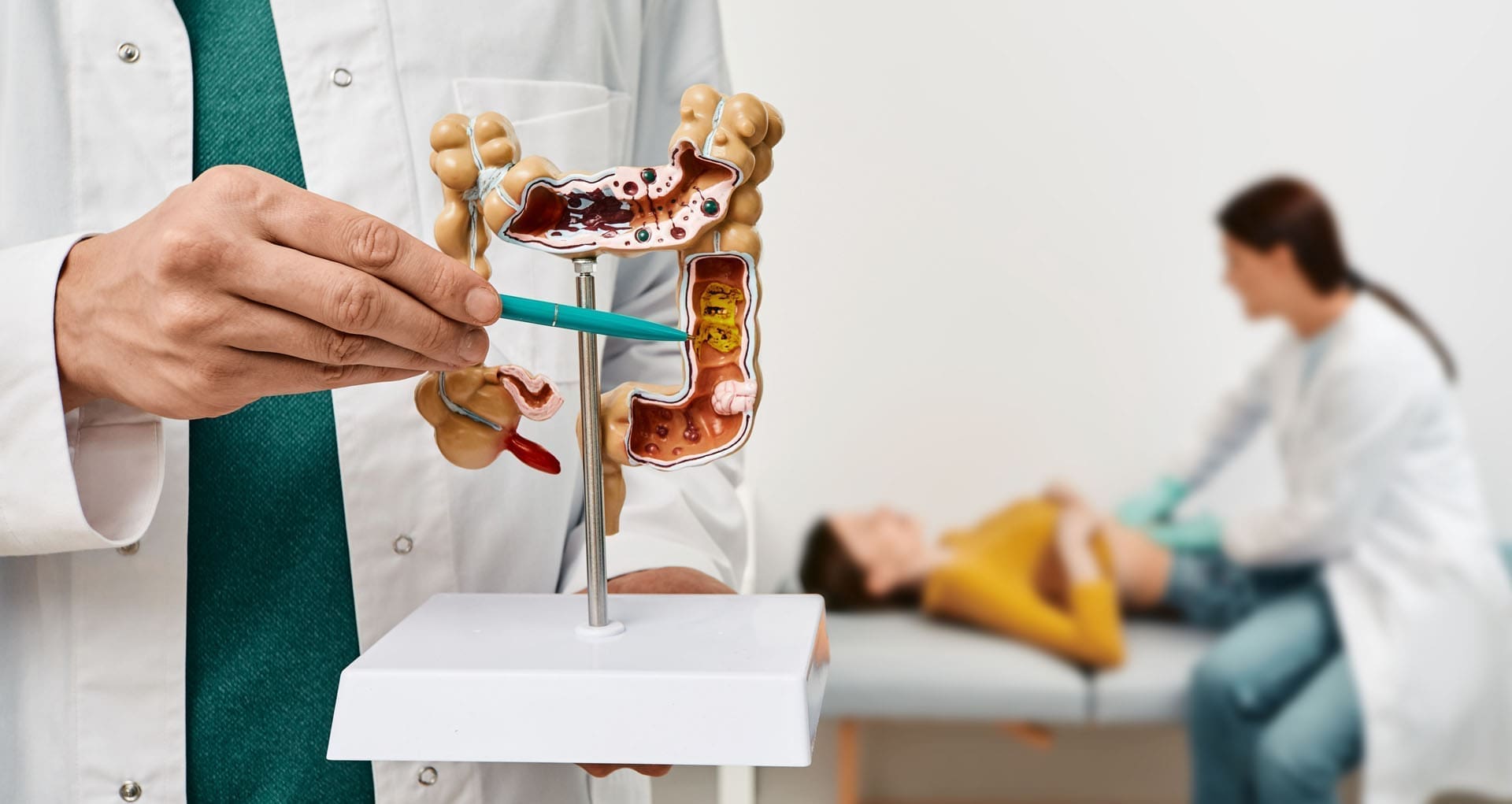
After a car crash, work injury, or sports accident, most people focus on pain, imaging, and therapy schedules. That makes sense. But your gut health also matters. The gut microbiome—the trillions of bacteria living in your intestines—affects digestion, inflammation, immune function, energy, and even mood. When this system becomes imbalanced (called dysbiosis), common problems like bloating, gas, irregular stools, and fatigue can get worse and slow recovery (Cleveland Clinic, 2024; Better Health Channel, 2023). Dysbiosis can be triggered by pain, stress, poor sleep, antibiotics, and a diet high in sugar and ultra-processed foods (USDA ARS, 2025; Cleveland Clinic, 2023).
This article explains dysbiosis in clear terms, shows how unhealthy bacteria gain the upper hand, and outlines simple steps to restore balance. It also describes how an integrated team—medical providers and chiropractors working together—can connect gut health to musculoskeletal care, imaging, and the medical-legal documentation often needed in personal-injury cases. Clinical observations from Alexander Jimenez, DC, APRN, FNP-BC (El Paso, TX) illustrate how a dual-scope approach helps real patients (Jimenez, n.d.; Jimenez, 2025).
What Is Dysbiosis?
Dysbiosis is an imbalance of gut bacteria—too many “unhelpful” species, not enough beneficial ones, or poor overall diversity (Cleveland Clinic, 2024). This shift can happen when:
- Diet is high in sugars and ultra-processed foods and low in fiber. Processed patterns “feed” invasive microbes and starve fiber-loving species (Cleveland Clinic, 2023).
- Medications like antibiotics kill harmful bacteria but also reduce helpful ones, opening space for overgrowth (Cleveland Clinic, 2024).
- Stress and sleep loss change gut motility and immune signaling through the gut–brain axis (Better Health Channel, 2023).
- Alcohol and environmental toxins further disrupt the microbiome and gut lining (USDA ARS, 2025).
Why it matters in injury care: dysbiosis may aggravate pain, fatigue, and inflammation, and it can complicate recovery if not addressed alongside physical treatment (Northwestern Medicine, n.d.).
How “Unhealthy” Bacteria Take Over
Unhealthy bacteria proliferate when the gut environment favors them. Three everyday drivers:
- Low-fiber, high-sugar, ultra-processed diet
Beneficial microbes thrive on plant fibers and resistant starches from beans, whole grains, vegetables, and fruit. When meals lack fiber and lean on refined carbs and additives, “good” bacteria lose ground (Cleveland Clinic, 2023; Healthline, n.d.). - Antibiotics and antimicrobial exposures
Antibiotics are often necessary (for example, for post-injury infections), but they can also disrupt the microbiome. Without healthy competitors, opportunistic strains may grow rapidly (Cleveland Clinic, 2024). - Stress and poor sleep
Stress hormones and short sleep disturb motility and increase gut permeability, which can push the biome toward dysbiosis (Better Health Channel, 2023).
Bottom line: the problem is conditions, not one single “bad bug.” Fix the conditions, and you help beneficial bacteria return.
SIBO: A Special Case to Know About
Small Intestinal Bacterial Overgrowth (SIBO) occurs when too many bacteria grow in the small intestine, an area that normally has low counts. SIBO can cause bloating, pain, diarrhea, and poor nutrient absorption. It may appear after surgeries or with motility issues—both can occur in complex injury cases (Mayo Clinic, 2024a).
Treatment can include antibiotics and diet strategies, but long-term success depends on identifying root causes (e.g., slow motility) and then rebuilding gut balance (Mayo Clinic, 2024b).
Why Gut Health Matters in Personal-Injury Care
- Inflammation and pain: A healthier microbiome produces short-chain fatty acids (SCFAs) like butyrate, which help protect the gut lining and may reduce systemic inflammation that worsens pain (DeGruttola et al., 2016).
- Energy and focus: Dysbiosis can relate to fatigue and brain fog, which can limit participation in physical therapy and home exercises (Northwestern Medicine, n.d.).
- Medication tolerance: If you need repeated or multiple medications, supporting the microbiome can reduce digestive side effects (Cleveland Clinic, 2024).
- Sleep and stress: Pain disturbs sleep; poor sleep worsens dysbiosis; dysbiosis feeds daytime fatigue—a cycle you want to break (Better Health Channel, 2023).
Clinical Insights from a Dual-Scope Practice (Dr. Alexander Jimenez, El Paso)
Alexander Jimenez, DC, APRN, FNP-BC, practices both chiropractic and nurse-practitioner medicine. In patients recovering from motor-vehicle accidents, work injuries, sports injuries, or chronic strain, his team coordinates:
- Dual-scope diagnosis: History, physical exam, neurologic and orthopedic testing, and when indicated, advanced imaging (X-ray/MRI) to clarify pain sources and rule out red flags (Jimenez, n.d.; Jimenez, 2025).
- Conservative therapies: Spinal adjustments when appropriate, soft-tissue work, targeted exercise, massage therapy, and acupuncture to improve mobility and calm the nervous system (Jimenez, 2025).
- Lifestyle and gut support: Plant-forward meal planning, fermented foods, sleep routines, and stress skills to support the microbiome while tissues heal (Penn State Health, 2018; Healthline, n.d.).
- Medical-legal documentation: Structured notes, outcome measures, and imaging reports to support claims and authorizations in personal-injury cases (Jimenez, n.d.).
Clinical correlation (Jimenez): Patients with spine pain, poor sleep, and high stress often report IBS-like flares. Combining manual therapy and graded exercise with a simple fiber-first plan and one fermented food daily often reduces bloating and meal-related discomfort within weeks—especially when sleep improves (Jimenez, 2025).
A Practical, Step-by-Step Gut-Reset for Injury Patients (4–6 Weeks)
Principle: Small, repeatable actions beat big, short-lived overhauls.
1) Make Plants the Base (Daily)
- Aim for variety: colorful vegetables and fruits, beans or lentils, and whole grains (oats, barley, quinoa, and brown rice).
- These foods feed beneficial bacteria and raise SCFAs that protect the gut lining (Ferranti, 2014).
2) Add One Fermented Food
- Choose yogurt or kefir with live cultures, or add kimchi/sauerkraut to bowls, tacos, or salads.
- Check labels for “live and active cultures.” Not all fermented foods have live microbes after processing (Healthline, n.d.; Cleveland Clinic Magazine, 2023).
3) Reduce Ultra-Processed Foods
- Swap sugary drinks for water or unsweetened tea.
- Choose whole-grain versions of staples.
- Keep packaged snacks as “sometimes foods,” not daily habits (Cleveland Clinic, 2023).
4) Support Sleep and Stress Management
- Keep a 7–9 hour sleep window.
- Try 5 minutes of slow breathing before bed (4–6 breaths/min).
- Add 20–30 minutes of walking most days; light strength 2–3 times/week (Better Health Channel, 2023).
5) Use Medications Wisely (With Your Clinician)
- Never stop a prescription on your own. If you need antibiotics or multiple meds, ask about food-first strategies and whether a probiotic is right for you (Cleveland Clinic, 2024).
6) Hygiene Matters
- Wash hands, rinse produce, and avoid cross-contamination to limit exposure to harmful bacteria (GoodRx, 2022).
7) Track Easy Wins
- Keep a 1-minute log: sleep hours, stress (0–10), fiber servings, and symptoms (bloating, stools, and energy). Look for trends over weeks, not days (Penn State Health, 2018).
Sample Injury-Friendly Meal Map (Budget-Minded)
- Breakfast: Oatmeal + kefir or yogurt + berries + nuts (fiber + live cultures).
- Lunch: Whole-grain bowl with beans/lentils + mixed veggies; spoonful of sauerkraut/kimchi.
- Dinner: Slow-cooker chili or lentil curry; side salad with olive oil and a baked potato (cool leftovers for resistant starch).
- Snacks: Fruit and nut butter, hummus and carrots, plain popcorn, and a small kefir smoothie.
These options are forgiving, inexpensive, and easy to repeat—exactly what most injury patients need during busy treatment weeks (Penn State Health, 2018).
Special Notes for SIBO or Sensitive Guts
If you have confirmed SIBO, some high-fiber or high-FODMAP foods may trigger symptoms early on. Under clinician guidance, some patients use a temporary limited plan, then gradually reintroduce fibers and fermented foods after treatment to prevent relapse (Mayo Clinic, 2024b). The goal is to avoid long-term restriction and build a resilient microbiome.
Coordinating Care in Personal-Injury Cases
At PersonalInjuryDoctorGroup.com, readers often need both health results and proper documentation:
- Care plans that link symptoms, exam findings, and imaging with diagnoses, procedures, and response to treatment.
- Clear records for insurers and attorneys: timelines, objective measures, and functional limitations.
- Return-to-work and activity guidance that matches recovery and prevents flare-ups.
An integrated medical–chiropractic clinic can provide the above while also addressing gut health so patients have better energy, sleep, and symptom control—key for completing rehab.
Red Flags: When to Seek Medical Care Now
- Unintended weight loss, blood in stool, fever, or severe pain.
- Night-time symptoms that wake you from sleep.
- History of GI surgery or inflammatory bowel disease.
Get evaluated promptly; discuss testing (including possible SIBO evaluation) and tailored treatment (Mayo Clinic, 2024a).
Key Takeaways
- Dysbiosis is common after injury due to stress, sleep loss, diet shifts, and medications—but it is fixable.
- Plant-forward eating, consuming one fermented food daily, reducing ultra-processed items, and improving sleep/stress care can steady digestion and support recovery.
- A dual-scope team (medical + chiropractic) can connect gut health with pain care, exercise therapy, imaging, and the documentation needed in personal-injury cases (Jimenez, 2025).
References
- Small intestinal bacterial overgrowth (SIBO) – Symptoms & causes. (2024a). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168
- Dysbiosis: What it is, symptoms, causes, treatment & diet. (2024). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/dysbiosis
- What is your gut microbiome? (2023). Cleveland Clinic. https://my.clevelandclinic.org/health/body/25201-gut-microbiome
- Gut health. (2023). Better Health Channel (Victoria State Government). https://www.betterhealth.vic.gov.au/health/healthyliving/gut-health
- Keeping a healthy gut. (2025). U.S. Department of Agriculture, Agricultural Research Service. https://www.ars.usda.gov/oc/utm/keeping-a-healthy-gut/
- Gut microbiome and health. (n.d.). Healthline. https://www.healthline.com/nutrition/gut-microbiome-and-health
- Gut check. (2023, Spring). Cleveland Clinic Magazine. https://magazine.clevelandclinic.org/2023-spring/gut-check
- The Medical Minute: Small changes make big differences in digestion. (2018). Penn State Health News. https://pennstatehealthnews.org/2018/03/the-medical-minute-small-changes-make-big-differences-in-digestion/
- DeGruttola, A. K., et al. (2016). Nutri-metabolic and microbiome cross-talk in inflammatory bowel diseases. World Journal of Gastroenterology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4947158/
- Small intestinal bacterial overgrowth (SIBO) – Diagnosis & treatment. (2024b). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/diagnosis-treatment/drc-20370172
- Good vs. bad bacteria—Gut health. (2022). GoodRx. https://www.goodrx.com/well-being/gut-health/good-bad-bacteria-gut-health
- Jimenez, A. (n.d.). Doctor of Chiropractic & Nurse Practitioner – Clinic resources. https://dralexjimenez.com/
- Jimenez, A. (2025). Professional profile and clinical insights. https://www.linkedin.com/in/dralexjimenez/
Post Disclaimers
General Disclaimer, Licenses and Board Certifications *
Professional Scope of Practice *
The information herein on "Gut Health Made Practical: Restore Your Balance" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic & Wellness Blog, where Dr. Alex Jimenez, DC, FNP-C, a Multi-State board-certified Family Practice Nurse Practitioner (FNP-BC) and Chiropractor (DC), presents insights on how our multidisciplinary team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those on this site and on our family practice-based chiromed.com site, focusing on naturally restoring health for patients of all ages.
Our areas of multidisciplinary practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is multidisciplinary, focusing on musculoskeletal and physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for musculoskeletal injuries or disorders.
Our videos, posts, topics, and insights address clinical matters and issues that are directly or indirectly related to our clinical scope of practice.
Our office has made a reasonable effort to provide supportive citations and has identified relevant research studies that support our posts. We provide copies of supporting research studies upon request to regulatory boards and the public.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: [email protected]
Multidisciplinary Licensing & Board Certifications:
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License #: TX5807, Verified: TX5807
New Mexico DC License #: NM-DC2182, Verified: NM-DC2182
Multi-State Advanced Practice Registered Nurse (APRN*) in Texas & Multi-States
Multi-state Compact APRN License by Endorsement (42 States)
Texas APRN License #: 1191402, Verified: 1191402 *
Florida APRN License #: 11043890, Verified: APRN11043890 *
Colorado License #: C-APN.0105610-C-NP, Verified: C-APN.0105610-C-NP
New York License #: N25929, Verified N25929
License Verification Link: Nursys License Verifier
* Prescriptive Authority Authorized
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card
Licenses and Board Certifications:
DC: Doctor of Chiropractic
APRNP: Advanced Practice Registered Nurse
FNP-BC: Family Practice Specialization (Multi-State Board Certified)
RN: Registered Nurse (Multi-State Compact License)
CFMP: Certified Functional Medicine Provider
MSN-FNP: Master of Science in Family Practice Medicine
MSACP: Master of Science in Advanced Clinical Practice
IFMCP: Institute of Functional Medicine
CCST: Certified Chiropractic Spinal Trauma
ATN: Advanced Translational Neutrogenomics
Memberships & Associations:
TCA: Texas Chiropractic Association: Member ID: 104311
AANP: American Association of Nurse Practitioners: Member ID: 2198960
ANA: American Nurse Association: Member ID: 06458222 (District TX01)
TNA: Texas Nurse Association: Member ID: 06458222
NPI: 1205907805
| Primary Taxonomy | Selected Taxonomy | State | License Number |
|---|---|---|---|
| No | 111N00000X - Chiropractor | NM | DC2182 |
| Yes | 111N00000X - Chiropractor | TX | DC5807 |
| Yes | 363LF0000X - Nurse Practitioner - Family | TX | 1191402 |
| Yes | 363LF0000X - Nurse Practitioner - Family | FL | 11043890 |
| Yes | 363LF0000X - Nurse Practitioner - Family | CO | C-APN.0105610-C-NP |
| Yes | 363LF0000X - Nurse Practitioner - Family | NY | N25929 |
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card






Comments are closed.