A herniated disc is typically a very painful condition, especially if the inner gel-like substance of the intervertebral disc, known as the nucleus pulposus, pushes through the thick, outer ring of cartilage and puts pressure on the sensitive nerves of the spine. Discs are soft, rubbery pads found between each vertebrae of the spine that act as shock-absorbers, allowing the spine to bend and/or flex. An intervertebral disc may begin to rupture as a result of wear-and-tear or due to a sudden injury. Fortunately, most individuals who’ve suffered a herniated disc can find relief from a variety of non-operative treatments before considering surgery. The following article highlights the impact of early treatment for herniated discs in the lumbar spine, or low back.
The Impact of Early Recovery on Long-Term Outcomes in a Cohort of Patients Undergoing Prolonged Non-Operative Treatment for Lumbar Disc Herniation: Clinical Article
Abstract
Object
The authors comprehensively studied the recovery of individual patients undergoing treatment for lumbar disc herniation. The primary goal was to gain insight into the variability of individual patient utility scores within a treatment cohort. The secondary goal was to determine how the rates and variability of patient recovery over time, represented by improvement in utility scores, affected long-term patient outcomes.
Methods
EuroQol Group–5 Dimension (EQ-5D) scores were obtained at baseline and at 2, 4, 8, 12, 26, 38, and 52 weeks for 93 patients treated under a prolonged conservative care protocol for lumbar disc herniation. Gaussian kernel densities were used to estimate the distribution of utility scores at each time point. Logistic regression and multistate Markov models were used to characterize individual patient improvement over time. Fisher exact tests were used to compare the distribution of EQ-5D domain scores.
Results
The distribution of utility scores was bimodal at 1 year and effectively sorted patients into a “higher†utility group (EQ-5D = 1; 43% of cohort) and a “lower†utility group (EQ-5D ≤ 0.86; 57% of cohort). Fisher exact tests revealed that pain/discomfort, mobility, and usual activities significantly differed between the 2 utility groups (p ≪ 0.001). The utility groups emerged at 8 weeks and were stable for the remainder of the treatment period. Using utility scores from 8 weeks, regression models predicted 1-year outcomes with 62% accuracy.
Conclusions
This study is the first to comprehensively consider the utility recovery of individual patients within a treatment cohort for lumbar disc herniation. The results suggest that most utility is recovered during the early treatment period. Moreover, the findings suggest that initial improvement is critical to a patient’s long-term outcome: patients who do not experience significant initial recovery appear unlikely to do so at a later time under the same treatment protocol.
Abbreviations used in this paper: AUC = area under a receiver-operating curve; EQ-5D = EuroQol Group–5 Dimension. Address correspondence to: Matthew C. Cowperthwaite, Ph.D., The University of Texas at Austin, Texas Advanced Computing Center, J.J. Pickle Research Campus, ROC 1.101, 10100 Burnet Rd., Austin, TX 78758. email: mattccowp@mac.com.
Plublished online June 28, 2013; DOI: 10.3171/2013.5.SPINE12992.
Introduction
Lumbar disc herniation is one of the most common causes of low-back pain and radiculopathy.[4] Treatment for patients with a herniated lumbar disc usually begins with conservative care such as analgesics, epidural steroid injections, and physical therapy,[1,5] with surgery reserved for patients with severe nerve root or cauda equina dysfunction or if conservative therapy is unsuccessful in controlling the symptoms.
Several recent studies have compared the effectiveness of conservative care and surgical treatment protocols for treating herniated lumbar discs, and have arrived at varying conclusions.[2,3,9,10,15–18] However, these studies have generally considered outcomes over a period of years, which is a significant length of time for patients who are waiting for their quality of life to improve. In clinical practice, this often leads to the following dilemma: most patients, particularly those with moderate symptoms, would prefer to avoid surgery, but are unwilling to wait an indefinite period of time for their symptoms to resolve. Unsurprisingly, lumbar discectomy is the most frequently performed surgical procedure in the US.[17,18]
Moreover, the above-mentioned studies have typically compared the average difference between treatment groups, without regard for individual recovery within the cohort. Additionally, this approach assumes that recovery in the protocols being compared proceeded similarly between observation intervals. To better understand the treatment responses of individual patients and the time frames of their responses, we comprehensively analyzed a cohort of patients undergoing a prolonged conservative care treatment protocol to gain insight into the dynamics of individual patient recovery over time, and whether these recovery dynamics influence long-term outcomes.
Methods
Study Data Set
The data set contained 142 patients randomized to a protocol of prolonged conservative care as part of the Leiden–The Hague Spine Intervention Prognostic Study.[10,15] The Sciatica Trial was reviewed and approved by the Medical Ethics Committee of Leiden University Medical Center.[11] Patients were enrolled into the Sciatica Trial entirely in the Netherlands.
In the Sciatica Trial, all patients aged 18 to 65 years, with persistent radicular pain in the L-4, L-5, or S-1 dermatome (with or without mild neurological deficit), severe disabling leg pain (lumbosacral radicular syndrome) lasting 6–12 weeks, and radiologically (MRI) confirmed disc herniation were considered eligible to enroll in the trial. Cauda equina syndrome or severe paresis, prior complaints of lumbosacral radicular syndrome in the previous 12 months, history of same-level unilateral disc surgery, spinal canal stenosis, and degenerative or lytic spondylolisthesis were all exclusion criteria. Cohort demographics and baseline characteristics were previously described; all patients reported both back and leg pain, but leg pain was generally more severe (mean leg pain 67.2 ± 27.7 vs back pain 33.8 ± 29.6, measured on a 100-point, horizontal visual analog scale).[15]
The Sciatica Trial used a pragmatic study design: conservative-care management was influenced as little as possible and was supervised by each patient’s general practitioner. Use of analgesics and physical therapy was determined by the treating physician. In this cohort, 46 patients (32%) elected to have surgery before the end of the 1st year; the mean timing of surgery was 12.6 weeks after the start of treatment. The surgical patients and 3 additional subjects with more than 2 missing utility measures were removed from the sample, resulting in a cohort of 93 patients considered in the present study; the crossover patients will be discussed in a separate study (manuscript in preparation). Our results were qualitatively unchanged when the excluded patients were retained in the analyses (data not shown).
In the Leiden–The Hague Spine Intervention Prognostic Study the EQ-5D instrument was used to measure patient utility at baseline and at 2, 4, 8, 12, 26, 38, and 52 weeks after enrollment into the study. The average duration of sciatica prior to enrollment was 9.5 weeks.[10,15] Utility is a valuation of a patient’s quality of life on a scale between 0 (as bad as dead) and 1 (perfect health). To estimate utility, the EQ-5D assesses a patient’s functional impairment in 5 domains: mobility, self-care, usual activities, pain, and anxiety.[6] For each domain, patients self-report the scores of 1 (no problems), 2 (some problems), or 3 (extreme problems). Utility scores were computed using the US valuation model,[12] which clearly distinguishes patients reporting no health problems (EQ-5D = 1) from those reporting at least some health problems (EQ-5D ≤ 0.86). Our results are independent of the particular valuation model (not shown). Completeness of the EQ-5D measures during follow-up ranged from 98% at 2 weeks to 90% at 38 weeks.
Statistical Analysis
All statistical analyses were conducted using the R statistical environment (version 2.9.2; www.rproject.org/) with the additional “msm,â€[8] “ROCR,â€[14] and “rmsâ€[7] packages (all freely available from cran.rproject.org). Continuous variables are presented as means (± SEM) and were compared using 2-tailed Student t-tests. Significance was assessed at an α ≤ 0.05 significance level, unless otherwise indicated. Missing EQ-5D measures were imputed using the mean of the measures at adjacent time points; our results are qualitatively similar under forward or backward imputation schemes (not shown).
Gaussian kernel density estimates were computed to estimate the distribution of utility scores. The kernel density estimates were estimated using a Silverman’s “rule-of-thumb†bandwidth and a Gaussian smoothing kernel.[13] The left- and right-most points were set to the theoretical minimum and maximum EQ-5D values, respectively, so that the area under the density curve summed to 1.
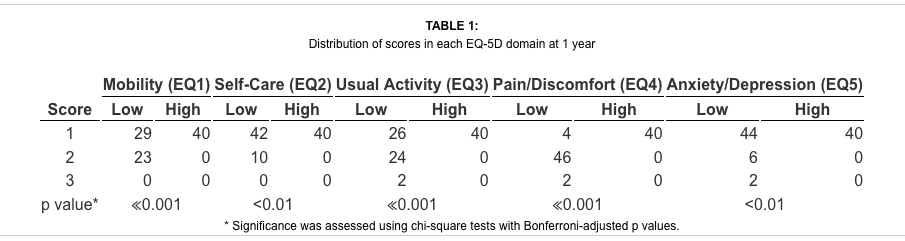
To determine whether specific EQ-5D domains differed between utility groups, Fisher-exact tests were conducted on contingency tables of the number of patients in each utility group that reported scores of 1, 2, or 3. Significance was assessed using a Bonferroni-corrected p value of 0.01.
Two-state, continuous-time Markov models were used to study the patterns and probabilities of patients transitioning between a “lower†utility (EQ-5D ≤ 0.86) and a “higher†utility group (EQ-5D = 1). The threshold utility value defining the groups remained fixed over time and was used to assign each patient to a utility group at each observation time. The models were fitted using the “msm†package[14] with piecewise-constant transition intensity matrices (Qt) estimated for each time interval between the points t = 0, 4, 8, 12, 26, 38, 52 (t = 2 was omitted because there were insufficient transitions to yield a robust model). Transition intensities were permitted to change between subsequent observation intervals, but remained homogeneous within each observation interval. The starting transition intensities were based on the observed frequencies of transitions in the data set and were calculated using the formula
![]()
in which nij is the observed number of transitions from Group i to Group j over the duration of the study period (T), and nj is the initial number of patients in Group j. The fitted models were robust to the choice of starting transition intensities and yielded qualitatively similar parameter estimates over a range of starting parameters (not shown). The likelihood function was maximized using a Nelder-Mead algorithm, and convergence was visually verified and typically occurred well short of the maximum number of iterations.
Logistic regression models were used to test whether utility measurements from earlier time points could predict long-term outcomes. These models only included utility values up to a particular time point as predictors, with the response variable being the patient’s 1-year outcome (higher or lower utility group) modeled as a dichotomous variable; no additional clinical or demographic covariates were included in the models. The models were fitted using the “rms†package[7] and the fit was assessed using chi-square tests (α ≤ 0.05). Separate regression models were created for all utility measurements up to and including those for 2, 4, 8, 12, and 26 weeks; for example, the 8-week model would include utility measurements at 0, 2, 4, and 8 weeks. The AUC statistic was used to assess the performance of the models and was calculated using the ROCR package.[14]
Results
Delineation of Higher and Lower Utility Groups
The distributions of patient utility scores markedly changed over the course of 1 year of conservative care (Fig. 1). At baseline, the majority of patients reported a relatively poor quality of life; the mean EQ-5D score was 0.55 (median 0.60). Two distinct utility groups were found to be present at baseline: a “lower†utility group (EQ-5D ≤ 0.86) and a “higher†utility group (EQ-5D = 1). At 6 months, the lower utility group (n = 62, 67%) was larger than the higher utility group (n = 31, 33%); at 1 year, the lower utility group (n = 53, 57%) had declined, but remained larger than the higher utility group (n = 40, 43%).
EQ-5D Domain Scores Between Groups
The average scores in each domain of the EQ-5D (Table 1) suggested that the pain/discomfort (low score = 1.9, high score = 1.0), mobility (low score = 1.4, high score = 1.0), and usual activities (low score = 1.5, high score = 1.0) domains differed most significantly between the high and low utility groups (p ≪ 0.001). The anxiety (low score = 1.2, high score = 1.0) and self-care (low score = 1.1, high score = 1.0) domains differed much less between the 2 utility groups, although they were also significant (p < 0.01).
Trajectory of Patient Utility Over Time
The series of patient utility scores measured over the study period are referred to as utility “trajectories,†which were studied to understand how patients recovered over the study period. In the study cohort, all patients experienced improvement during at least 1 observation period; only 19.3% (n = 18) never experienced a decline during their recovery. Recovery was variable: 49.5% of the patients (n = 46) experienced at least 2 reversals, which were defined as improvements (declines) immediately followed by declines (improvements) at the next observation. Furthermore, only 29% of patients (n = 27) had stable trajectories with no reversals. Overall, increases in utility were 4 times more common than decreases in utility.
The utility of the entire cohort increased by 0.296 (51.8% above baseline; p ≪ 0.001, Wilcoxon Mann-Whitney test) over the year (Fig. 2), but was markedly faster during the first 2 months (0.022/week) than the final 3 months (0.005/week). Over the same time frames, utility scores improved by 0.178 (35.2% above the baseline average) over the first 2 months and by 0.063 (1.3% above the 9-month average) during the final 3 months. The mean utility scores significantly differed between the 2 final utility groups at 8 weeks and remained significant for the rest of the year (p < 0.01, Student t-test; Fig. 2).
Modeling Patient Recovery
Given that 2 utility groups were present over the study period, Markov models were used to study the robustness of these groups by estimating the likelihood of patients switching between the groups. The models suggested that the average probability of a patient remaining within their utility group was 97.9% and 97.6% for patients currently in the low and high utility groups, respectively (Fig. 3). The probability of a patient transitioning from the low to the high utility group was 2.1%; the corresponding probability for transitions from the high to the low utility group was 2.3%.
The models also suggested that the likelihood of a patient transitioning to another utility group declined over the study period. During the first 8 weeks, 2.8% and 3.5% of patients experienced low-to-high and high-to-low transitions, respectively; over the last 3 months, 1.6% and 1.3% of patients experienced low-to-high and high-to-low group transitions, respectively.
Predicting Individual Patient Outcome
At 8 weeks, logistic regression models could predict a patient’s outcome (final utility group) with modest accuracy (AUC = 0.62, or 62%). The accuracy of the models steadily increased as data from later time points were included; the 26-week model performance was good with an AUC of 0.78 (Fig. 4). The amount of improvement in utility scores from baseline to 8 weeks was also investigated as a predictor of good outcome (higher utility group). Patients with EQ-5D scores that improved by at least 0.30 during the first 8 weeks of treatment were 60% more likely to have a good outcome.
Dr. Alex Jimenez’s Insight
Herniated disc commonly develop in the lumbar spine, or lower back. Also referred to as a slipped disc or a ruptured disc, a herniated disc occurs when the soft, gel-like center of an intervertebral disc pushes through a tear in its surrounding outer ring, known as the annulus fibrosus. The symptoms of a herniated disc are generally specific to the exact level of the spine where the disc herniation occurs and whether or not the nerve tissue has been irritated by the intervertebral disc material leaking out of the inside of the disc. The most common symptoms of a disc herniation include pain, numbness, weakness and tingling sensations as well as causing radiating symptoms along the upper or lower extremities. Depending on the severity of the symptoms, herniated disc treatment can include, drugs and/or medications, epidural injections, physical therapy, chiropractic, and surgery, among others. According to the following article, early treatment can help promote and manage a faster herniated disc recovery from prolonged non-operative treatment methods.
Discussion
Several studies have sought to compare the relative effectiveness of surgery and conservative care for treatment of a lumbar disc herniation.[4–9,11] Generally, these studies have compared “average†differences between the study cohorts, while the individual trajectories by which patient utility changes over time have received less attention. To our knowledge, this study provides the first comprehensive statistical analysis of individual patient-level utility data from a large cohort of patients randomized to a prolonged conservative-care treatment protocol for lumbar disc herniation.[9]
The decision to proceed with surgery is straightforward in patients with severe, disabling symptoms or neurological deficits. Likewise, the decision to continue conservative care is simple for patients with mild symptoms or those who are content to live with their symptoms indefinitely. However, patients with moderate symptoms often present a greater challenge because most patients would prefer to avoid surgery if possible, but are also not content to wait indefinitely for their pain to resolve. These patients often ask for more than just the overall probability they will improve eventually; they usually want to know when they will recover. Moreover, they are usually interested in whether their current symptoms and progress affect the probability and extent of their future improvement.
For patients with moderate symptoms, the following observations from our study may be useful. First, the utility scores for individual patients diverged sharply at 8 weeks and were thereafter easily classified as either those reporting no health problems (higher utility, EQ-5D = 1) or those reporting at least some health problems (lower utility, EQ-5D ≤ 0.86). Among the lower utility group, the “pain/discomfort,†“mobility,†and “usual activities†domains of the EQ-5D differed most significantly from the higher utility group, which could potentially represent incompletely treated radiculopathy. Second, most improvement occurred early: almost one-third of the overall improvement in utility came in the first 2 months, while only 1% occurred in the last 3 months. Third, recovery is variable, with most patients (80%) experiencing at least 1 interval of deterioration and only 19% continuously improving without any setbacks. This may provide some reassurance to patients with generally good recovery to “stay the course†without resorting to more invasive measures such as surgery simply because of what may be a brief transient decrease in quality of life. Lastly, the probability of moving into another group was quite low (2%), which may be considered when counseling a patient who is not improving with his or her current treatment regimen.
We note the following limitations inherent in this cohort study. First, this is an observational study, and therefore we cannot infer causality for the emergence of the 2 utility groups, and because the individual treatment plans were unknown to us, we cannot comment on any specific type of conservative therapy. However, even if one considers the patients in the low utility group as nonresponders to conservative therapy (which is likely at least partly incorrect), the study does not imply that surgery would necessarily be beneficial in these patients. Second, the EQ-5D scores a patient’s overall health, and therefore unknown comorbid conditions likely account for at least some of the patients residing in the lower utility group and for part of the utility fluctuations. However, in the clinical setting, it should be obvious as to whether a patient’s symptoms are resulting from unresolved radiculopathy or from preexisting comorbidities. Lastly, we excluded crossover patients from our analysis. Crossover patients are likely those with the most severe symptoms and thus our results may be limited to patients with mild to moderate symptoms. However, we believe this exclusion is appropriate because, as mentioned above, the decision to operate is fairly straightforward when a patient has severe symptoms. From a clinical standpoint, patients with moderate symptoms and without neurological deficits after 8 weeks need the most information about the potential time course and extent of their nonoperative recovery to make an informed treatment decision.
The focus of the present study is individual utility recovery within a patient cohort rather than comparing average response to different treatment protocols. The goal was to gain insight into the dynamics of utility recovery among individual patients treated conservatively, but our approach could be applied to almost any treatment protocol. Studies of the changes (improvements or declines) in individual utility over time are useful because they may provide insights into a patient’s perception of their current treatment protocol (for example, patients in the low utility group would likely report a poor response to treatment), and also to identify a point at which continuing the same treatment is unlikely to improve a patient’s quality of life. Patients entering a conservative-care treatment protocol are likely to experience an initial period of rapid recovery, followed by a longer phase of more modest recovery. Our results suggest that, once the long-term recovery phase begins, patients are unlikely to spontaneously change their recovery for better or worse under the same treatment protocol. Lastly, patient utility scores early in the treatment process were reasonable predictors of long-term outcomes. This study is a comprehensive characterization of individual patients’ recovery of health utility from a lumbar disc herniation, and provides a unique picture for clinicians taking care of these patients. Our findings suggest that most recovery occurs early during treatment, and this early recovery period is important to long-term outcomes.
Conclusions
In a cohort of patients undergoing prolonged conservative care for treatment of lumbar disc herniation, 57% of the patients had lingering health problems at 1 year. Utility was recovered most rapidly early in the treatment process, and the majority of utility was also recovered in the initial treatment period. After the initial recovery period, we could identify with reasonable accuracy those patients who would fully recover and those who would not. Over the course of the year, recovery was observed to be highly variable, although most fluctuations were relatively small and only transient. These findings suggest that patients not initially responding to their treatment protocol should consider other options because they are unlikely to respond at a later time. However, patients and clinicians should also be mindful of transient decreases in quality of life, and carefully consider any changes in their treatment plan.
Disclosure
This work was partially supported by a charitable grant from the St. David’s Foundation Impact Fund to Dr. Cowperthwaite, and does not necessarily represent the views of the Impact Fund or the St. David’s Foundation.
Author contributions to the study and manuscript preparation include the following. Conception and design: all authors. Acquisition of data: Cowperthwaite, van den Hout. Analysis and interpretation of data: all authors. Drafting the article: Cowperthwaite. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Cowperthwaite. Statistical analysis: Cowperthwaite, van den Hout. Administrative/technical/material support: Cowperthwaite. Study supervision: Cowperthwaite.
In conclusion, early non-operative treatment of lumbar herniated disc can effectively improve as well as manage recovery outcomes in patients with the condition. It’s important for patients with disc herniations in the lumbar spine to comprehend the source of their issue before receiving appropriate treatment for their symptoms. Furthermore, non-operative treatment is effective in most patients, surgical interventions may be considered according to the individual’s recovery outcome. Information referenced from the National Center for Biotechnology Information (NCBI). The scope of our information is limited to chiropractic as well as to spinal injuries and conditions. To discuss the subject matter, please feel free to ask Dr. Jimenez or contact us at 915-850-0900 .
Curated by Dr. Alex Jimenez
1. Andersson GB, Brown MD, Dvorak J, Herzog RJ, Kambin P, Malter A, et al.: Consensus summary of the diagnosis and treatment of lumbar disc herniation. Spine (Phila Pa 1976) 21:24 Suppl75S–78S, 1996 Medline
2. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al.: The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976) 21:1777–1786, 1996 Crossref, Medline
3. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, Long JM, et al.: The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 21:1787–1795, 1996 Crossref, Medline
4. Baldwin NG: Lumbar disc disease: the natural history. Neurosurg Focus 13:2E2, 2002
5. Dawson E, Bernbeck J: The surgical treatment of low back pain. Phys Med Rehabil Clin N Am 9:489–495, x, 1998
6. EuroQol Group: EuroQol—a new facility for the measurement of health-related quality of life. The EuroQol Group Health Policy 16:199–208, 1990 Crossref, Medline
7. Harrell FE: Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression and Survival Analysis New York, Springer, 2001
8. Jackson CH, Sharples LD, Thompson SG, Duffy SW, Couto E: Multistate Markov models for disease progression with classification error. The Statistician 52:193–209, 2003
9. Keller RB, Atlas SJ, Singer DE, Chapin AM, Mooney NA, Patrick DL, et al.: The Maine Lumbar Spine Study, Part I. Background and concepts. Spine (Phila Pa 1976) 21:1769–1776, 1996 Crossref, Medline
10. Peul WC, van den Hout WB, Brand R, Thomeer RTWM, Koes BW: Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ 336:1355–1358, 2008 Crossref, Medline
11. Peul WC, van Houwelingen HC, van der Hout WB, Brand R, Eekhof JA, Tans JT, et al.: Prolonged conservative treatment or ‘early’ surgery in sciatica caused by a lumbar disc herniation: rationale and design of a randomized trial [ISRCT 26872154]. BMC Musculoskelet Disord 6:8, 2005 Crossref, Medline
12. Shaw JW, Johnson JA, Coons SJ: US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care 43:203–220, 2005 Crossref, Medline
13. Silverman BW: Density Estimation for Statistics and Data Analysis London, Chapman & Hall, 1986
14. Sing T, Sander O, Beerenwinkel N, Lengauer T: ROCR: visualizing classifier performance in R. Bioinformatics 21:3940–3941, 2005
15. van den Hout WB, Peul WC, Koes BW, Brand R, Kievit J, Thomeer RTWM, et al.: Prolonged conservative care versus early surgery in patients with sciatica from lumbar disc herniation: cost utility analysis alongside a randomised controlled trial. BMJ 336:1351–1354, 2008 Crossref, Medline
16. Weber H: Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976) 8:131–140, 1983 Crossref, Medline
17. Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson ANA, et al.: Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA 296:2451–2459, 2006 Crossref, Medline
18. Weinstein JN, Tosteson TD, Lurie JD, Tosteson ANA, Hanscom B, Skinner JS, et al.: Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA 296:2441–2450, 2006 Crossref, Medline
1. Anurekha Ramakrishnan, MS, K. Michael Webb, MD, and Matthew C. Cowperthwaite, PhD. (2017) One-year outcomes of early-crossover patients in a cohort receiving nonoperative care for lumbar disc herniation. Journal of Neurosurgery: Spine 27:4, 391-396. . Online publication date: 1-Oct-2017. Abstract | Full Text | PDF (2037 KB)
2. Kimberly A Plomp, Una Strand Viðarsdóttir, Darlene A Weston, Keith Dobney, Mark Collard. (2015) The ancestral shape hypothesis: an evolutionary explanation for the occurrence of intervertebral disc herniation in humans. BMC Evolutionary Biology 15:1. . Online publication date: 1-Dec-2015. [Crossref]

Additional Topics: Neck Pain
Neck pain is a common complaint which can result due to a variety of injuries and/or conditions. According to statistics, automobile accident injuries and whiplash injuries are some of the most prevalent causes for neck pain among the general population. During an auto accident, the sudden impact from the incident can cause the head and neck to jolt abruptly back-and-forth in any direction, damaging the complex structures surrounding the cervical spine. Trauma to the tendons and ligaments, as well as that of other tissues in the neck, can cause neck pain and radiating symptoms throughout the human body.

IMPORTANT TOPIC: EXTRA EXTRA: A Healthier You!
OTHER IMPORTANT TOPICS: EXTRA: Sports Injuries? | Vincent Garcia | Patient | El Paso, TX Chiropractor
Post Disclaimers
Professional Scope of Practice *
The information herein on "Amazing Results from Herniated Disc Early Treatment | El Paso, TX" is not intended to replace a one-on-one relationship with a qualified health care professional or licensed physician and is not medical advice. We encourage you to make healthcare decisions based on your research and partnership with a qualified healthcare professional.
Blog Information & Scope Discussions
Welcome to El Paso's Premier Wellness and Injury Care Clinic blog, where Dr. Alex Jimenez, DC, FNP-C, a board-certified Family Practice Nurse Practitioner (FNP-C) and Chiropractor (DC), presents insights on how our team is dedicated to holistic healing and personalized care. Our practice aligns with evidence-based treatment protocols inspired by integrative medicine principles, similar to those found on dralexjimenez.com, focusing on restoring health naturally for patients of all ages.
Our areas of chiropractic practice include Wellness & Nutrition, Chronic Pain, Personal Injury, Auto Accident Care, Work Injuries, Back Injury, Low Back Pain, Neck Pain, Migraine Headaches, Sports Injuries, Severe Sciatica, Scoliosis, Complex Herniated Discs, Fibromyalgia, Chronic Pain, Complex Injuries, Stress Management, Functional Medicine Treatments, and in-scope care protocols.
Our information scope is limited to chiropractic, musculoskeletal, physical medicine, wellness, contributing etiological viscerosomatic disturbances within clinical presentations, associated somato-visceral reflex clinical dynamics, subluxation complexes, sensitive health issues, and functional medicine articles, topics, and discussions.
We provide and present clinical collaboration with specialists from various disciplines. Each specialist is governed by their professional scope of practice and their jurisdiction of licensure. We use functional health & wellness protocols to treat and support care for the injuries or disorders of the musculoskeletal system.
Our videos, posts, topics, subjects, and insights cover clinical matters, issues, and topics that relate to and directly or indirectly support our clinical scope of practice.*
Our office has reasonably attempted to provide supportive citations and has identified the relevant research studies or studies supporting our posts. We provide copies of supporting research studies available to regulatory boards and the public upon request.
We understand that we cover matters that require an additional explanation of how they may assist in a particular care plan or treatment protocol; therefore, to discuss the subject matter above further, please feel free to ask Dr. Alex Jimenez, DC, APRN, FNP-BC, or contact us at 915-850-0900.
We are here to help you and your family.
Blessings
Dr. Alex Jimenez DC, MSACP, APRN, FNP-BC*, CCST, IFMCP, CFMP, ATN
email: coach@elpasofunctionalmedicine.com
Licensed as a Doctor of Chiropractic (DC) in Texas & New Mexico*
Texas DC License # TX5807
New Mexico DC License # NM-DC2182
Licensed as a Registered Nurse (RN*) in Texas & Multistate
Texas RN License # 1191402
ANCC FNP-BC: Board Certified Nurse Practitioner*
Compact Status: Multi-State License: Authorized to Practice in 40 States*
Graduate with Honors: ICHS: MSN-FNP (Family Nurse Practitioner Program)
Degree Granted. Master's in Family Practice MSN Diploma (Cum Laude)
Dr. Alex Jimenez, DC, APRN, FNP-BC*, CFMP, IFMCP, ATN, CCST
My Digital Business Card




 Again, I Welcome You.
Again, I Welcome You.
Comments are closed.